Katie Meyers
Compendium Review Seven – Reproduction
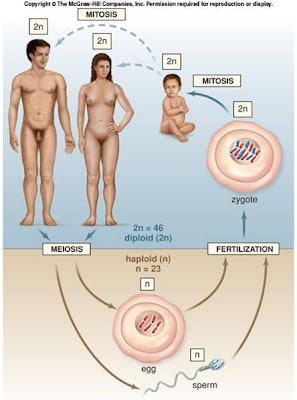
Human Life Cycle
- Overview of events in human life cycle
- Aging
Reproductive Organs (Genitals)
- 5 functions
- Male reproductive system
- Overview of male reproductive organs
- Steps of male reproductive system
- Ejaculation
- Testes
- Female reproductive system
- Organs
- External genitals
- Meiosis
- Female hormones
- Uterine cycle – non-pregnant
- Ovarian cycle – non-pregnant
- Uterine and ovarian cycles – pregnant
- Menopause
Birth Control Options, Infertility, and STDs
- Birth Control – some examples
- Infertility
- STDs – sexually transmitted diseases
- Viral
- Bacterial
- Prevention
Fetal Development at Birth
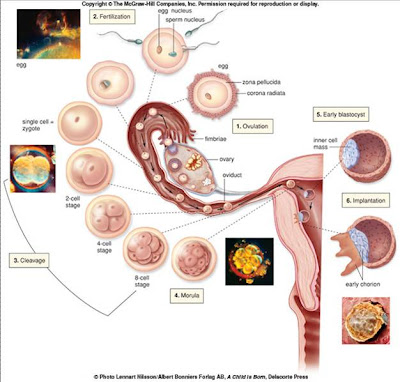
- Fertilization
- Implantation
- Processes of Development
- Extraembryonic membranes
- Development stages
- Pre-embryonic development
- Embryonic development
- Fetal development
- Genital development
- Pregnancy and birth
- Parturition
- Placenta
- Mother/fetus blood never mixes
- Umbilical cord
- Maternal changes in female anatomy
- How mother can prevent birth defects
- Birth
- 3 stages
- Many different approaches
Human Life Cycle
- Overview of events in human life cycle (in order)
- Meiosis
- “Reduction division”
- Occurs only in sex organs
- Fertilization
- Fetal Development
- Birth
- Childhood/Adolescence
- Puberty – when a child becomes, by a series of event, a sexually competent adult
- Reproductive system does not fully function until puberty is complete
- Occurs…
- 11 – 13 in females
- 14 – 16 in males
- Adulthood
- (found on slide 4 of Reproduction – BIO 156 PowerPoint presentation)
- During this stage, adults’ sex organs perform meiosis in preparation of having children
- Aging
- Death
- Changes to each of these stages is due to the aging process
Reproductive Organs (Genitals)
- 5 functions
- 1)
- Males – produce sperm within testes
- Females – produce eggs within ovaries
- 2)
- Males – nurture, transport, and eject sperm
- Females – transport eggs to uterus
- 3)
- Males – penis delivers sperm to…
- Females – …vagina – takes in sperm, ejects menstrual fluid, is birth canal
- 4)
- Females – uterus allows fertilized egg to develop and be nourished within a female
- Females – breasts provide nourishment after birth
- 5)
- Both – testes/ovaries produce respective sex hormones
- These hormones bring about masculinization/feminization
- Females – allow pregnancy to continue
- During sexual intercourse, both male and female will ideally experience orgasms
- Male Reproductive System
- (Overview of) Male Reproductive Organs
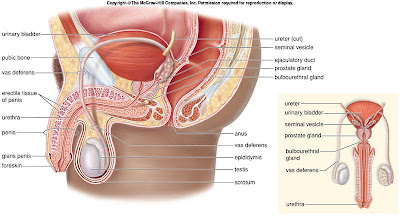
- (found on slide 6 of Reproduction – BIO 156 PowerPoint presentation)
- Testes – produce sperm and sex hormones; primary sex organ; plural (there are two)
- Millions of sperm in just a few drops of testicular fluid
- Scrotum – sacs that suspend testes (two of them)
- Epididymides – ducts; store sperm; this is where sperm also matures
- Vasa deferentia – conduct and store sperm
- Seminal vesicles – contribute nutrients and fluid to semen
- Prostate gland – contributes fluid to semen
- Urethra – conducts sperm
- Bulbourethral glands – contribute fluid containing mucous to semen
- Penis – sexual intercourse organ
- Prepuce – part of penis; removed during circumcision
- Steps of the male reproductive system
- Sperm is produced in left and right testes
- The vas deferens (left, right) carry it up into the abdominal cavity
- At base of penis, it (sperm) joins with urethra
- Semen produced by prostate and seminal glands at the penis’s base
- Ejaculation occurs
- When sperm travel from testes, are joined by semen, and ejected through erect penis
- At time of ejaculation, sperm leaves penis by means of semen
- 3 types of vesicles/glands add secretions to seminal fluid (see above: seminal vesicles, prostate gland, bulbourethral glands)
- Seminal fluid
- Each component is different and has a particular function
- Basic solution (more viable)
- Sugar fructose (provide sperm with energy)
- Prostaglandins (chemicals that contract uterus, moving sperm toward egg)
- Testes
- Begin developing inside abdominal cavity, descend into scrotal sacs during last two months of fetal development
- Scrotum regulates their temperature by holding them closer/farther from body, depending on their current temperature and the environment
- Each composed of…
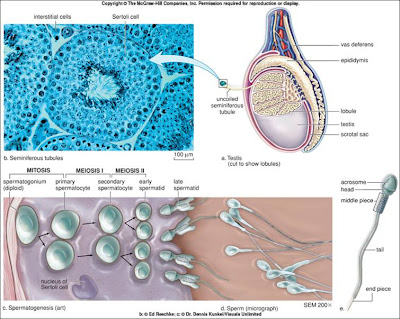
- (found on slide 7 of Reproduction – BIO 156 PowerPoint presentation)
- Lobules
- Contain one to three seminiferous tubules
- Packed with cells undergoing spermatogenesis (production of sperm) by meiosis
- Seroti cells support, nourish, and regulate spermatogenesis
- Sperm not ejaculated is reabsorbed by testicular tissue
- It takes approximately 74 days for sperm to develop from spermatogenesis into sperm
- Mature sperm (spermatozoa) – 3 parts
- Head – nucleus covered by acrosome (which stores enzymes to penetrate egg)
- Middle piece – has mitochondria that provide energy for tail movement
- Tail – flagellum
- Do not live more than 48 hours in female genital tract
- Interstitial cells
- Live between seminiferous tubules
- Secrete sex hormone
- Most important sex hormone is testosterone
- (found at http://www.andrologyaustralia.org/images/pageContentImages/MI_Image_Jul2005_04.jpg)
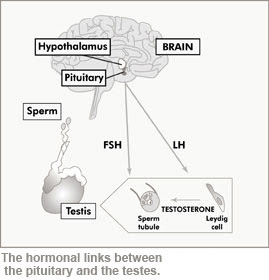
- Hypothalamus controls testes’ sexual function
- Secretes hormone gonadotropin – releasing hormone (GnRH)
- 2 types
- Follicle-stimulating hormone (FSH)
- Luteinizing hormone (LH)
- Used in negative feedback relationship; maintains fairly constant production of sperm and testosterone
- Female Reproductive System
- Organs
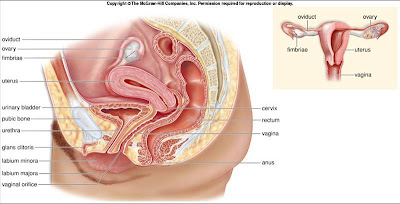
- (found on slide 9 of Reproduction – BIO 156 PowerPoint presentation)
- Ovaries – produce eggs (oocytes) and sex hormones (estrogen and progesterone)
- Site of initial meiosis, where unfertilized eggs are produced
- Oviducts – conduct eggs; location of fertilization in uterine/fallopian tubes specifically; lined with cilia
- Uterus (womb) – houses developing fetus
- Placenta – sustains development of embryo/fetus
- Cervix – contains opening to uterus
- Hysterectomy – removal of cervix; a form of sterilization
- Vagina – receives penis during sexual intercourse
- Birth canal
- Exit for menstrual flow
- Acidic environment
- External genitals
- Collectively known as the vulva
- 2 labia majora (folds of skin)
- Mons pubis
- Labia minora – similar to labia majora, just closer to vagina
- Urethra and vagina openings inside labia minora
- Glans clitoris
- Hymen – partially closes vagina; ring of tissue (virginity)
- Meiosis
- Occurs in ovaries
- Phase One
- Occurs in fetal ovary
- One egg per month (ovulation part of menstrual cycle) matures and bursts from ovarian wall and taken up into the fallopian tube
- Phase Two
- Occurs moment egg is fertilized, if that even happens
- Possibly very large gap between phases
- Female hormones
- Ovaries’ production of hormones
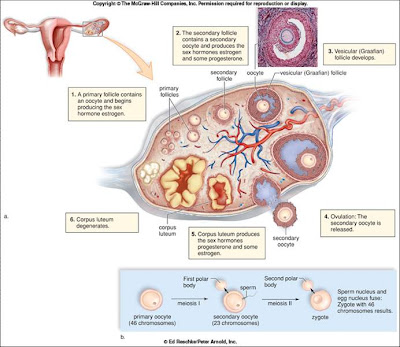
- (found on slide 10 of Reproduction – BIO 156 PowerPoint presentation)
- Primary follicles – produce estrogen
- Secondary follicles – produce estrogen and some progesterone
- Corpus luteum – produces progesterone
- Hypothalamus – same function in females as in males
- Hormone secretion (GnRH, FSH, LH) not constantly present, but secreted at different rates during menstrual cycle
- Estrogen – responsible for secondary female sex characteristics, e.g. body hair, fat distribution
- Estrogen and progesterone both required for breast development
- Uterine cycle – non-pregnant – average 28-day cycle
- Menstruation – days 1-5
- Endometrium breaks down
- Proliferative phase – days 6-13
- Endometrium rebuilds
- Secretory phase – days 15-28
- Endometrium thickens
- Glands become secretory
- Ovarian cycle – non-pregnant – average 28-day cycle (occurs simultaneously with uterine cycle)
- Follicular phase – days 1-13
- Follicle maturation occurs
- Estrogen secretion prominent
- Ovulation – day 14
- LH spike occurs
- Luteal phase – days 15-28
- LH secretion occurs
- Corpus luteum forms
- Progesterone secretion prominent
- Here is a picture of both the uterine and ovarian non-pregnant cycles
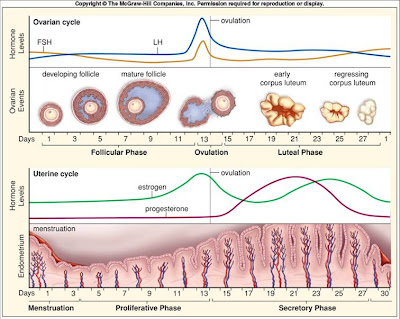
- (found on slide 11 of Reproduction – BIO 156 PowerPoint presentation)
- Here is a picture of both the uterine and ovarian pregnant cycles – unlike non-pregnant cycle, progesterone does not drop (because it helps maintain uterus wall in preparation of pregnancy)
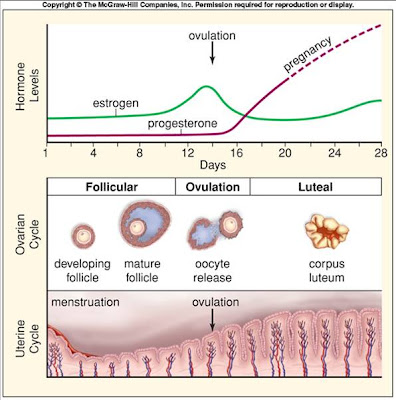
- (found on slide 12 of Reproduction – BIO 156 PowerPoint presentation)
- Menopause – when ovarian cycle stops
- Begins between the ages of 45 and 55
Birth Control Options, Infertility, and STDs
- Birth Control – some examples
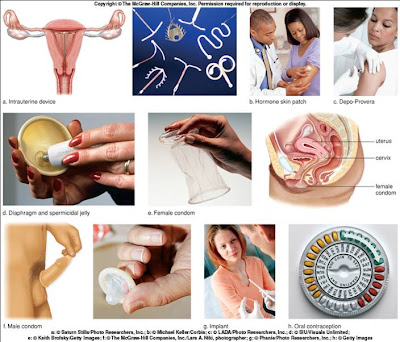
- (found on slide 13 of Reproduction – BIO 156 PowerPoint presentation)
- Abstinence – most reliable
- Prevents transmission of STDs
- Family planning – on of the least effective options
- 70% family planners succeed with the program
- Specifically female
- Contraceptives – medications, e.g. birth control pills
- Contraceptive implants – capsule that utilizes synthetic progesterone, prevents ovulation
- Contraceptive injections – either progesterone only or a progesterone/estrogen mix
- From a few weeks to three months between shots
- Contraceptive vaccines – immunize woman to hormones associated with egg production, e.g. HCG
- “Morning-after pills” – emergency contraception
- Intrauterine device (IVD) – small molded plastic piece inserted into uterus by physician
- Mostly inhibits fertilization
- Makes implanting impossible
- Diaphragm – soft latex cup with flexible rim
- Lodges behind pubic bone, fits over cervix
- Individually fitted
- Used with spermicidal jelly or cream
- Put in no more than two hours before sexual activity
- Remove at least six hours after sexual activity
- Female condom – large polyurethane tube
- Open end has ring that covers external genitals
- Considered a barrier method
- Renewed interest in STD protection possibility
- Tubal ligation – cuts and seals oviducts
- Brings about sterilization
- Should be considered permanent
- Specifically male
- Male condom – latex sheath goes over erect penis
- Better form of protection if used with spermicide
- Same as female condom in that it is considered a barrier method
- Renewed interest in STD protection possibility
- Vasectomy – cuts and seals vas deferens
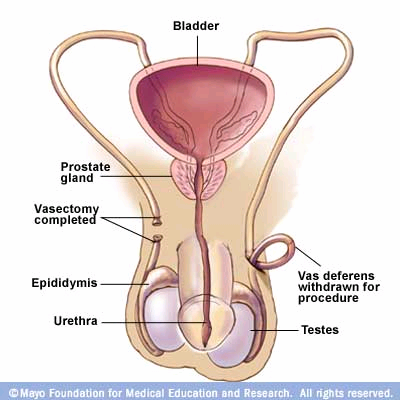
- (found on slide 8 of Reproduction – BIO 156 PowerPoint presentation)
- Form of sterilization
- Should be considered permanent
- Infertility
- Definition – failure of a couple achieving pregnancy after one year of effort (unprotected, regular intercourse)
- Estimated 15% of couples infertile
- 40% -- males; low sperm count or much abnormal sperm
- 40% -- females; body weight
- 20% -- both
- Assisted reproductive technologies
- Artificial Insemination by Donor – sperm placed into vagina by physician
- In Vitro Fertilization – conception in lab glassware
- Gamete Intrafallopian Transfer – similar to IVF
- Eggs removed and reintroduced in same procedure/time period
- Surrogate mothers – paid women bring stranger’s baby to term
- Intracytoplasmic sperm injection
- Used in sever male fertility problems
- One sperm directly injected into egg
- STDs – sexually transmitted diseases
- Viral – none curable yet
- HIV infection – fatal
- Genital warts
- Caused by human papillomavirus (HPV)
- Genital herpes
- Caused by herpes simplex virus
- Type One – cold sores, fever blisters
- Type Two – genital herpes
- Above two very common and uncomfortable
- Hepatitis
- Infects liver by failure, cancer, or death
- Easily transmittable
- No immediate consequences
- ABCDEG
- A – not sexually transmitted; fecal to mouth
- BCDEG – transmitted by…
- Sexual contact
- Contaminated blood
- B – most common sexually transmitted hepatitis; can lead to liver failure
- CDEG – liver cancer possibilities; no vaccines yet available
- Bacterial – curable with antibiotics
- Chlamydia
- Gonorrhea – 40% strains now resistant to antibiotic therapy
- Syphillis – 3 stages
- Bacterial vaginosis (BV)
- Responsible for about 50% of vaginitis in American women
- “Caused by a disruption of the normal flora in the vagina leading to an overgrowth of certain bacteria” (from slide 16 of Reproduction – BIO 156 PowerPoint presentation)
- Candida albicans
- Overgrowth of normal yeast in vagina
- Characterized by – tissue that is red, inflamed, itchy; with, curdy discharge sometimes too
- Women using birth control hormones/antibiotics more prone
- Trichomonas vaginalis
- Caused by a type of protozoan
- Causes – frothy discharge, foul smell, itching
- Common cause of vaginitis
- Ways to prevent STD transmission
- Abstinence
- Long-term monogamous relationship(s)
- Be aware of partner’s STD history and risky (STD-wise) behavior
- Practice safe sex
Fetal Development and Birth
- Fertilization – union of sperm and egg resulting in zygote
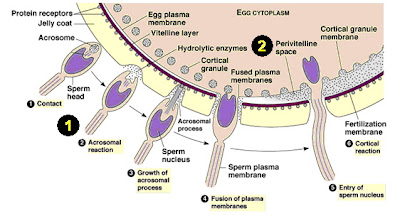
- (found at http://www.bio.davidson.edu/Courses/Molbio/MolStudents/spring2005/Dresser/sperm%20and%20egg%20fusion.jpg)
- Flagellum on sperm finds (swims towards) egg
- Sperm head only (nucleus) fuses with egg’s nucleus
- Zygote receives cytoplasm and organelles from mother only
- Approximately one week from fertilization to implantation
- During that week, only mitosis occurs
- Implantation
- Normally in uterine wall
- Ectopic pregnancy – when a fertilized egg implants before getting to uterine wall, e.g. oviduct
- Can be dangerous, lead to hemorrhaging
- First step to take if pregnancy is suspected – find where zygote implanted
- Processes of Development
- Cleavage – occurs during mitotic cell division of the zygote
- Growth – cell division accompanied by daughter cells becoming larger
- Morphogenesis – shaping of the embryo
- First evident when some cells move/migrate compared to the other cells – such movements make embryo assume various shapes
- Differentiation – when cells take on specific structure and/or function
- Extraembryonic membranes
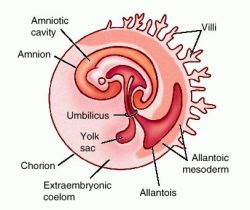
- (found at http://img.tfd.com/dorland/thumbs/amnion.jpg)
- Outside embryo
- 4 types
- Chorion – develops into fetal half of placenta
- Allantois – extends away from embryo
- Deal with kidneys/urinary tract and has umbilical blood vessels
- Yolk sac – first to appear of the four
- Contains many blood vessels – first site of blood cell formation
- Amnion – enlarges relative to embryo/fetus
- Contains cushioning fluid to protect embryo/fetus
- Overview of early embryonic development (about first month)
- “Basic body plan laid down”
- “No organs formed”
- “Placenta develops”
- “Very little growth, fetus still tiny”
- Above quotes from slide 20 of Reproduction – BIO 156 PowerPoint presentation
- Development Stages
- Pre-embryonic development
- Contains the events of the first week
- Zygote division while traveling down oviduct to uterus
- (found on slide 19 of Reproduction – BIO 156 PowerPoint presentation)
- Embryonic development

- (from slide 20 of Reproduction – BIO 156 PowerPoint presentation)
- Goes from second week to end of second month
- Week two – embryo begins implanting in uterus
- Gastrulation occurs
- Turns inner cell mass into embryonic disk
- An example of morphogenesis
- At completion, there is…
- 3 primary germ layers
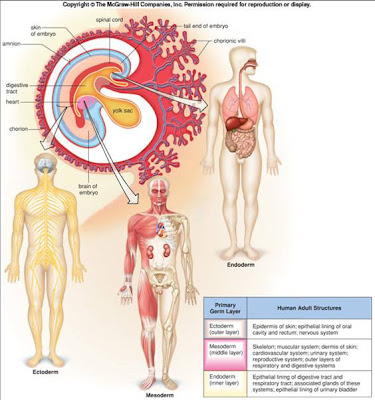
- (found on slide 21 of Reproduction – BIO 156 PowerPoint presentation)
- Ectoderm
- Mesoderm
- Endoderm
- Embryonic disk has become embryo
- Week three – two important organ systems appear
- Nervous system
- Heart (both third and fourth weeks)
- Week four – body stalk (future umbilical cord) connect embryo to chorion; limb buds (flippers) appear
- Week five – head enlarges; sense organs gain prominence; visual development (possible to see) of eyes, ears, and nose
- Week six to week eight – embryo changes into recognizable human being; head achieves normal relationship with body; neck region develops; nervous system responsive (to reflex actions); all organ systems established
- Fetal development – fetus is recognizably human
- Month three – fingernails appear; gender distinguishable by ultrasound
- Month four – skeleton visible; hair begins appearing; cartilage begins being replaced by bone
- Month five – heartbeat heard; vernix caseosa (cheesy protective coating) begins being deposited; mother begins feeling movment – pregnancy obvious
- Month six – body covered with lanugo (fine hair); wrinked and reddish skin
- Month seven – testes descend into scrotum; eyes are open; possible for baby to survive if born now
- Month eight – body hair begins disappearing; depositing of subcutaneous fat begins
- Month nine – fetus ready for birth and about 20 ½ inches long and 7 ½ pounds
- Male and female development of genitals
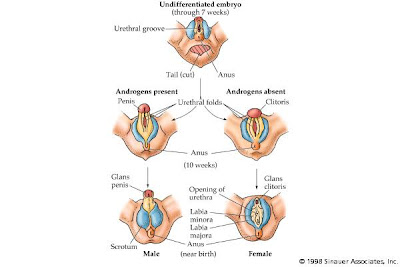
- (found at http://www.mie.utoronto.ca/labs/lcdlab/biopic/fig/41.13.jpg)
- Development of gonads and ducts, development of external genitals
- Sex of fetus determined at fertilization
- Males – XY
- Male XX syndrome
- Females – XX
- Female XY syndrome
- Both syndromes result in ambiguous sex determination
- Gonads do not start developing until the seventh week
- At six weeks, males and females have same types of ducts
- At fourteen weeks, primitives testes/ovaries are located deep inside abdominal cavity
- Pregnancy and birth
- Parturition – process of birthing offspring
- Placenta – source of progesterone and estrogen during pregnancy
- 2 sides
- Fetal side – contributed by chorion
- Maternal side – consisting of uterine tissue
- Placental hormones cause…
- Fluctuations in energy levels
- Uterus relaxation
- Pulmonary values to increase
- Stress incontinence
- Decreased venous return
- Edema
- Varicose veins
- Stretch marks (Striae gravidarum)
- Peptide hormone (from placenta) brings about pregnancy-induced diabetes
- Mother/fetus blood never mixes
- (found at http://images.main.uab.edu/healthsys/ei_0181.gif)
- Umbilical cord – fetus’s lifeline
- Contains umbilical arteries and vein
- Maternal changes in female anatomy
- Shift in organs
- Bladder and rectum pushed superiorly and squeezed, resulting in changes in urination and defecation patterns
- Stomach is compressed, making the mother eat more often, but less at every meal
- Appetite change due to immune response changing to avoid possible poisons for the fetus’s sake
- “Postural changes to compensate for anterior weight” (found on slide 22 of Reproduction – BIO 156 PowerPoint presentation)
- Breasts enlarge because of milk production
- First milk production begins around the sixth month of pregnancy
- How mother can prevent birth defects
- Get a physical exam
- Have good health habits
- Avoid…
- Drinking alcohol
- Smoking cigarettes
- Taking illegal drugs
- Taking medications not approved by your physician
- Exposure to environmental toxins and radiations
- Help prevent conditions associated with birth
- Birth
- 3 stages
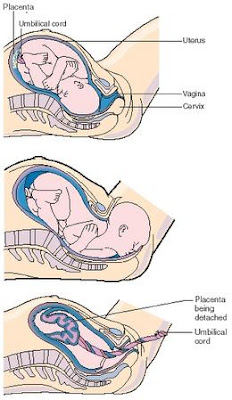
- (found at http://www.scienceclarified.com/images/uesc_02_img0089.jpg)
- Stage One
- Effacement – taking up the cervix – done by uterine contractions
- Amniotic membrane ruptures, if it has not already
- First stage of parturition ends once cervix is completely dilated
- Stage Two
- Beings when uterine contractions occur every one to two minutes and last about one minute each
- Mother has desire to push, or bear down
- As soon as head is delivered physician may hold head and guide it downward
- After birth, umbilical cord is cut and tied once baby is breathing normally and functioning independently
- Stage Three
- Afterbirth (placenta) is delivered about 15 minutes after delivery
- Many different approaches to the birthing and the child-raising processes

No comments:
Post a Comment